A mental health assessment intake form template streamlines the process of gathering essential patient information. It ensures accurate documentation of symptoms, medical history, and personal background. Utilizing standardized templates improves clinical efficiency and supports effective treatment planning.
Mental Health Assessment Intake Form Template Sample PDF Viewer
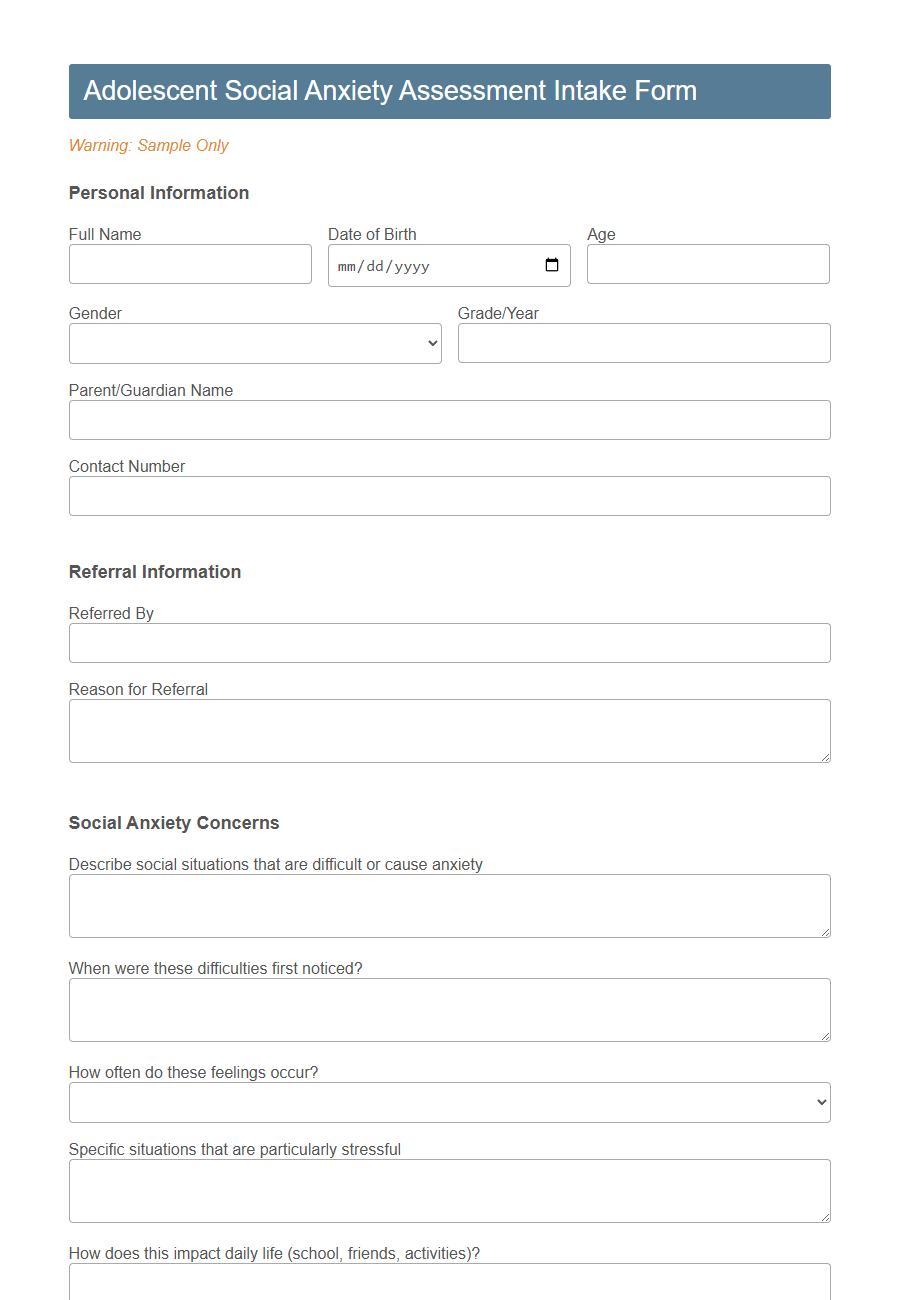
Image example of Mental Health Assessment Intake Form Template:
Mental Health Assessment Intake Form Template Samples
Adolescent Social Anxiety Assessment Intake - PDF - HTML
Trauma-Informed Teletherapy Intake - PDF - HTML
Perinatal Mental Health Assessment Intake - PDF - HTML
Geriatric Cognitive Screening Intake - PDF - HTML
Military Veteran PTSD Intake - PDF - HTML
First Responder Mental Health Intake - PDF - HTML
Eating Disorders Initial Assessment Intake - PDF - HTML
Autism Spectrum Disorder (ASD) Adult Intake - PDF - HTML
ADHD Adult Diagnostic Intake - PDF - HTML
Substance Use Dual Diagnosis Intake - PDF - HTML
Chronic Pain and Mental Health Intake - PDF - HTML
Child Play Therapy Intake - PDF - HTML
Introduction to Mental Health Assessment Intake Forms
Mental Health Assessment Intake Forms are essential tools used by clinicians to gather comprehensive information about a client's psychological well-being.
These forms help in identifying symptoms, medical history, and personal background to create a tailored treatment plan. Accurate intake forms ensure effective communication between the client and mental health professional from the beginning of therapy.
Importance of Intake Forms in Mental Health Care
Mental health assessment intake forms are essential tools that gather comprehensive information about a patient's psychological history, symptoms, and current mental state. These forms help clinicians create accurate diagnoses and personalized treatment plans by providing a structured way to document critical mental health data. Efficient use of intake forms enhances communication between patients and mental health professionals, leading to improved care outcomes.
Key Components of a Mental Health Assessment Intake Form
A Mental Health Assessment Intake Form is essential for gathering comprehensive client information at the start of therapy.
Key components include personal identification details, such as name, age, and contact information, to ensure accurate record-keeping. It also covers presenting issues and reasons for seeking mental health support to understand the client's concerns clearly.
Medical history and current medications are vital to identify any physical health factors impacting mental health. Mental health history, including previous diagnoses and treatments, helps in creating an effective treatment plan.
Assessment of current symptoms and emotional state provides insight into the client's mental health status and immediate needs. Risk assessment questions evaluate any potential harm to self or others, ensuring safety throughout care.
Social and family history sections reveal environmental influences and support systems relevant to the client's well-being. Lifestyle factors, such as substance use and daily habits, offer additional context for accurate diagnosis and intervention.
Goal setting allows clients and clinicians to establish clear objectives for therapy, promoting motivation and focused progress. Consent and confidentiality statements confirm understanding and agreement with treatment policies, protecting client rights throughout the therapeutic process.
Essential Personal Information Fields
A Mental Health Assessment Intake Form Template gathers crucial personal details to provide effective care. Essential personal information fields ensure accurate identification and tailored treatment plans.
- Full Name - Records the individual's legal name for clear identification and documentation.
- Date of Birth - Captures age-related information to support age-appropriate interventions.
- Contact Information - Includes phone number and email to enable communication and appointment coordination.
Collecting these fundamental details creates a solid foundation for comprehensive mental health evaluation and support.
Medical and Psychiatric History Section
The Medical and Psychiatric History section of a Mental Health Assessment Intake Form Template gathers essential background information to understand a patient's overall health. This section helps clinicians identify past medical issues and psychiatric conditions that may influence current mental health.
- Comprehensive medical history - Records chronic illnesses, surgeries, medications, and allergies relevant to mental health treatment.
- Psychiatric diagnoses and treatments - Documents previous mental health diagnoses, hospitalizations, and therapy or medication interventions.
- Family psychiatric history - Captures mental health conditions among close relatives to assess genetic or environmental risk factors.
Symptoms and Presenting Concerns Checklist
What symptoms are you currently experiencing that affect your daily life? Please describe any emotional, physical, or behavioral changes you have noticed recently.
Which presenting concerns are most troubling to you at this time? Identifying these helps tailor the assessment to address your specific needs.
Risk Assessment and Safety Screening
The Mental Health Assessment Intake Form Template includes a detailed Risk Assessment and Safety Screening section to identify any immediate dangers or self-harm tendencies. This section helps clinicians gather crucial information about suicidal thoughts, substance abuse, and potential harm to others. Early identification of these risks ensures timely intervention and appropriate support for the client's safety and well-being.
Confidentiality and Consent Considerations
The Mental Health Assessment Intake Form Template prioritizes patient confidentiality and clear consent protocols to protect sensitive information. This approach ensures trust and compliance with legal and ethical standards.
- Confidentiality Commitment - The form clearly outlines how personal information will be securely stored and who has authorized access.
- Informed Consent - Clients are provided with detailed explanations of the assessment process and must explicitly agree before proceeding.
- Limits of Confidentiality - The form specifies situations where confidentiality may be legally breached, such as risk of harm or court orders.
Customizing Your Mental Health Intake Form Template
Customizing your mental health assessment intake form template allows you to gather essential, personalized information that meets the specific needs of your practice and clients. Tailoring questions to reflect the unique aspects of your therapy approach enhances the accuracy and relevance of the data collected.
Incorporate fields that address client history, current symptoms, and treatment goals to create a comprehensive and effective intake form.
