Medication reconciliation forms ensure accurate tracking of patient prescriptions, minimizing errors during care transitions. Examples of these forms highlight essential components like current medications, allergies, and dosage instructions. Proper use of these templates facilitates safer medication management and improved patient outcomes.
Medication Reconciliation Form Sample PDF Viewer
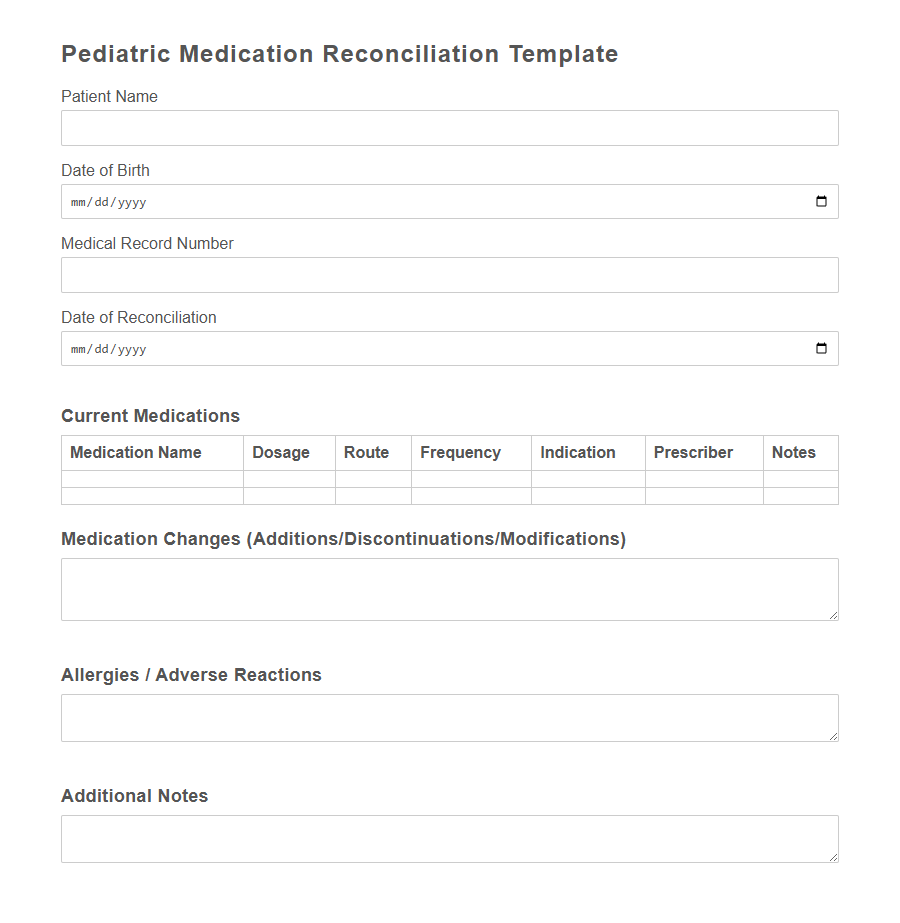
Image example of Medication Reconciliation Form:
Medication Reconciliation Form Samples
Pediatric Medication Reconciliation Template - PDF - HTML
Hospital Admission Medication Reconciliation Form - PDF - HTML
Discharge Medication Reconciliation Checklist - PDF - HTML
Outpatient Clinic Medication Reconciliation Document - PDF - HTML
Long-Term Care Facility Medication Reconciliation Sheet - PDF - HTML
Emergency Department Medication Reconciliation Record - PDF - HTML
Home Health Medication Reconciliation Worksheet - PDF - HTML
Specialty Pharmacy Medication Reconciliation Template - PDF - HTML
Behavioral Health Medication Reconciliation Form - PDF - HTML
Oncology Clinic Medication Reconciliation Sheet - PDF - HTML
Pre-Operative Medication Reconciliation List - PDF - HTML
Telemedicine Medication Reconciliation Form - PDF - HTML
Post-Transplant Medication Reconciliation Template - PDF - HTML
Geriatric Medication Reconciliation Checklist - PDF - HTML
Anticoagulation Clinic Medication Reconciliation Document - PDF - HTML
Introduction to Medication Reconciliation Forms
Medication reconciliation forms are essential tools used in healthcare to ensure accurate and complete medication information is communicated across transitions of care.
These forms help prevent medication errors by providing a clear and updated record of all medications a patient is taking. Proper use of medication reconciliation forms improves patient safety and enhances the quality of care.
Importance of Accurate Medication Records
Accurate medication records are crucial for patient safety and effective treatment.
They prevent medication errors, such as duplications, omissions, or harmful drug interactions, by providing healthcare providers with a clear and complete history of a patient's medications. Maintaining precise records ensures continuity of care across different medical settings and supports informed clinical decisions.
Key Components of a Medication Reconciliation Form
A Medication Reconciliation Form is essential for ensuring accurate and comprehensive medication management during patient care transitions. It helps prevent medication errors by compiling a complete list of a patient's current medications.
Key components of the form include patient identification details, a current medication list, and any documented allergies or adverse reactions.
Steps in the Medication Reconciliation Process
What are the initial steps in the medication reconciliation process? The first step involves collecting a complete and accurate list of the patient's current medications from multiple sources. This ensures all prescribed, over-the-counter, and herbal products are accounted for.
How is the medication list verified during reconciliation? Healthcare providers compare the collected list against the physician's orders to identify any discrepancies. This verification helps prevent medication errors and ensures patient safety.
What happens after identifying discrepancies in the medication list? The next step is to resolve any discrepancies through communication with the healthcare team and the patient. Clarifications ensure the final medication list is accurate and up to date.
How is the finalized medication list documented? The complete, verified medication list is recorded in the patient's medical record using the medication reconciliation form. Proper documentation supports continuity of care and future reference.
What follow-up actions are taken after medication reconciliation? Regular updates and reviews of the medication list occur at every transition of care to maintain accuracy. Continuous monitoring helps to reduce the risk of adverse drug events.
Common Errors in Medication Documentation
Common errors in medication documentation include incorrect drug names, dosages, and frequencies, which can lead to serious patient safety risks. Omissions of prescribed medications or failure to update medication changes contribute to incomplete records. Accurate and thorough medication reconciliation forms are essential to prevent adverse drug events and ensure effective patient care.
Roles and Responsibilities in Medication Reconciliation
Medication reconciliation forms ensure accurate and complete medication information is documented to prevent errors during patient care transitions. Clear roles and responsibilities are essential for effective medication reconciliation.
- Healthcare Providers' Responsibility - Verify and document the patient's current medications accurately during admission, transfer, and discharge.
- Pharmacists' Role - Review medication histories and reconcile discrepancies to ensure patient safety and medication effectiveness.
- Nurses' Duty - Communicate patients' medication information and changes to the care team to support continuity of care.
Electronic vs. Paper-Based Reconciliation Forms
Electronic Medication Reconciliation Forms enhance accuracy by reducing manual errors and enabling real-time updates in patient medication records. Paper-Based Forms, while familiar and easy to implement, often lead to inefficiencies and increased risk of incomplete or outdated information. Transitioning to electronic systems supports better communication among healthcare providers and improves overall patient safety.
Best Practices for Effective Medication Reconciliation
Accurate medication reconciliation is essential for ensuring patient safety and preventing medication errors. Implementing best practices can streamline the process and improve clinical outcomes.
- Comprehensive Data Collection - Gather complete medication histories from multiple sources, including patients, pharmacies, and previous medical records.
- Standardized Documentation - Use a uniform medication reconciliation form to ensure consistency in recording and reviewing patient medications.
- Interdisciplinary Collaboration - Involve healthcare professionals across disciplines to verify and update medication lists effectively.
Impact on Patient Safety and Outcomes
Medication Reconciliation Forms are essential tools for ensuring accurate and complete medication information transfer between healthcare providers. They significantly reduce the risk of medication errors, improving overall patient safety and clinical outcomes.
- Prevents Medication Errors - These forms help identify and rectify discrepancies in medication lists, minimizing adverse drug events.
- Enhances Communication - They provide a standardized method for healthcare professionals to share up-to-date medication information.
- Improves Patient Outcomes - Accurate medication reconciliation supports effective treatment plans and reduces hospital readmissions.
Implementing thorough Medication Reconciliation Forms is critical for safeguarding patient health and enhancing care quality.
